The nose is a defining feature of the face.Under such intense scrutiny, it’s no shock that many of us feel dissatisfied with the features we are judged on most heavily – our noses. After all, they’re often one of the first things people notice when they look at you. Thanks to medical advancements, rhinoplasty offers a safe and effective way to enhance the aesthetics of your nose. A skilled rhinoplasty surgeon like Dr. Rizk can seamlessly straighten a crooked or off-center nose1, reduce the size of an overly large nose, remove bumps or humps2 on the bridge of the nose, change the shape of the tip, narrow nostrils that are too wide and even raise or lower the height of the nasal bridge. Beyond aesthetics, rhinoplasty can help improve breathing by reshaping or repositioning internal structures such as the septum or turbinates.
The results of rhinoplasty can often be highly transformational and even life-changing. There are many different types of noses and common concerns3 people have about the shape or size of their nose. No matter what your unique concerns may be, Dr. Rizk can help you achieve a nose that is aesthetically pleasing and proportionate to your facial features.
Different Types of Noses | Nose Shapes
The modern human nose is a complex and intricate part of our anatomy, and its shape varies highly between different people. The shape of a nose is determined by the nasal bones and cartilage that form its structure. There are several different types of noses, each with their own distinct features:
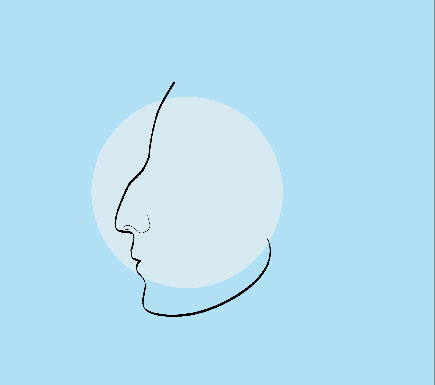
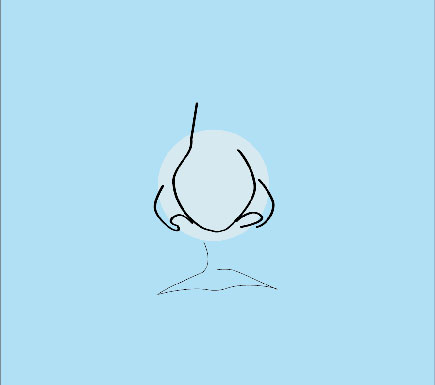
Roman Nose
The Roman Nose is characterized by a straight bridge that has a slight bump in the middle. It often has a wide nostril opening and can be found in Mediterranean and Latin American populations.

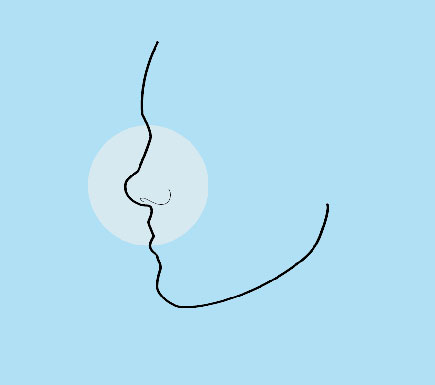
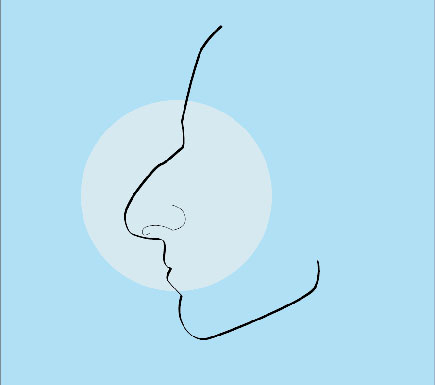
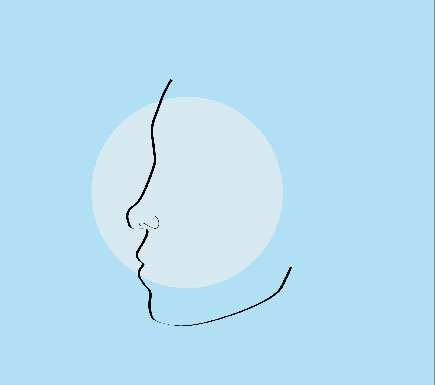
Greek Nose
The Greek Nose has a curved bridge and long, narrow nostrils. It is most commonly seen in people of Caucasian descent.
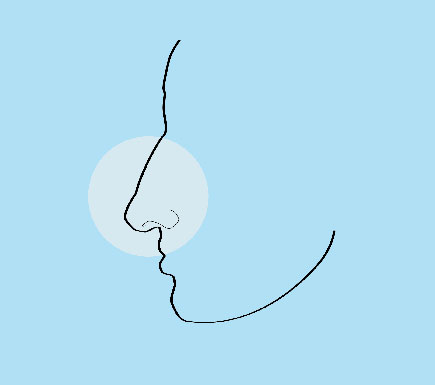
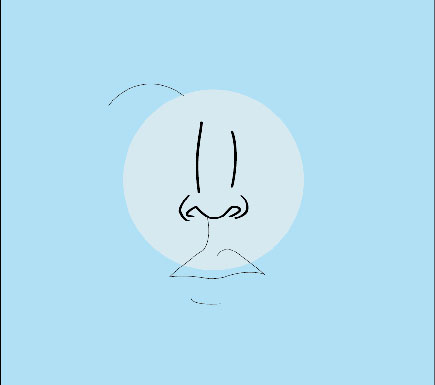
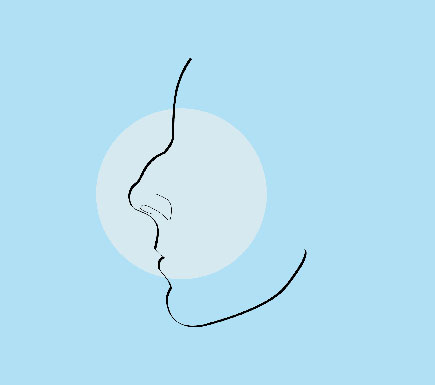
Snub Nose
The Snub Nose is identified by its upturned shape, with the tip of the nose pointing upwards toward the sky. It can be seen in many different ethnicities.
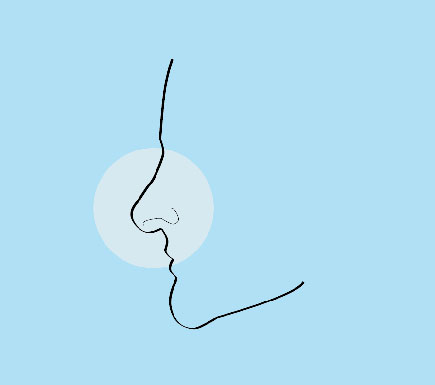
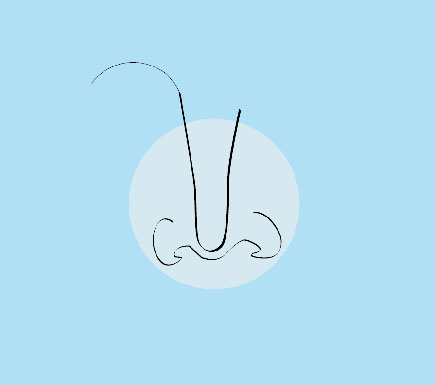
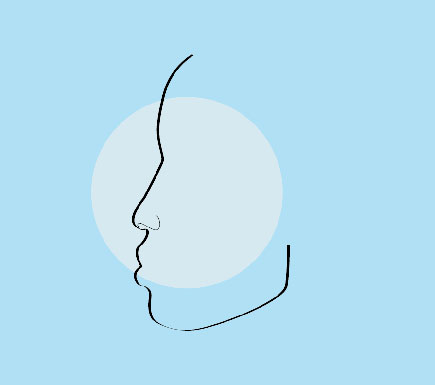
Hook Nose
The Hook Nose has a curved bridge, with the tip of the nose pointing downwards toward the ground. It is often found among Mediterranean and Middle Eastern populations.
Button Nose
The Button Nose is characterized by its short length and small size. This type of nose is often seen in Asian and Scandinavian populations.
Aquiline Nose
The Aquiline Nose has a hooked bridge, with the tip of the nose pointing downwards towards the ground. It is commonly seen in African and Indian populations.
Common Nose Concerns
A drooping nose occurs when the tip of your nose droops downwards towards your upper lip. This usually happens due to aging and can be corrected with cosmetic surgery.
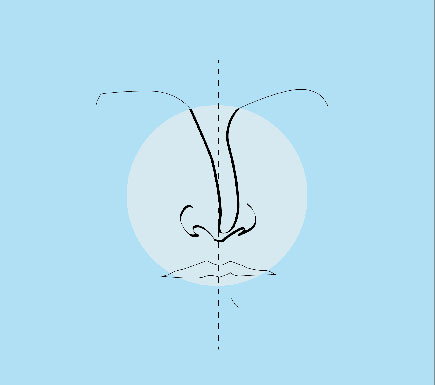
A wide nose is a condition where the nostrils are wider than what is considered normal or attractive. This can be caused by genetics, trauma, or other factors. It can be corrected through surgery or with the use of filler injections.
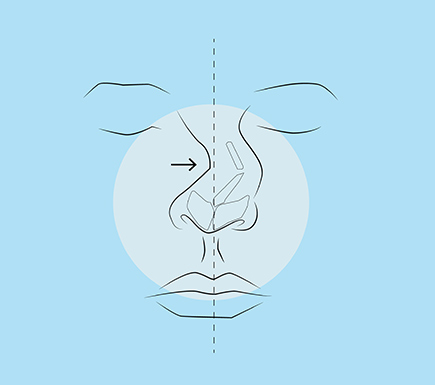
A deviated septum is a condition where the partition between your nostrils is not straight, causing one side to appear larger than the other. This can obstruct breathing and cause difficulty in airflow, which can be treated by corrective surgery.
A broken nose, also known as a nasal fracture, may be caused by a direct impact to the face. Common causes of this type of injury include falls, sports injuries, physical fights and car accidents.
An upturned nose is a condition where the tip of your nose bends upwards. This can be caused by genetics or trauma, and can be corrected through surgery.
A bulbous nose is a condition when the nasal tip appears round and enlarged. This can be corrected through rhinoplasty surgery or by using injectable fillers.
A pinched tip nose is a condition where the tip of your nose appears squeezed or compressed. This can be corrected through rhinoplasty surgery.
A wide nose bridge is a condition where the bridge of your nose appears wider than normal. This problem can be remedied with surgery.
If the size of your nose is not in proportion with the rest of your facial features, it can be corrected through rhinoplasty surgery. This procedure can be used to make the nose smaller, depending on your desired outcome.
If the size of your nose is too small, this can be corrected with fillers or surgery. Fillers are temporary and will need to be replaced periodically to maintain the desired size, whereas surgery is a more permanent solution.
A crooked nose is a condition where the bridge of your nose appears crooked or bent. This can be due to genetics or trauma, and can be corrected through rhinoplasty surgery.
A hump on the nose is a condition where there is a bump or ridge on the bridge of the nose. This can be due to genetics or trauma, and can be corrected through rhinoplasty surgery.
A flat nose is a condition where the bridge of your nose appears flattened or depressed.
An asymmetrical nose is a condition where the two sides of your nose appear different from each other in terms of size or shape.
Hooked Nose
A hooked nose is a condition where the bridge of your nose is curved and the tip points downwards. It can be seen in many ethnicities and can be corrected through surgery.
Snub Nose
A snub nose is a condition where the bridge of your nose appears shortened and curved inwards.
Long Nose
A long nose is a condition where the bridge of your nose appears elongated.
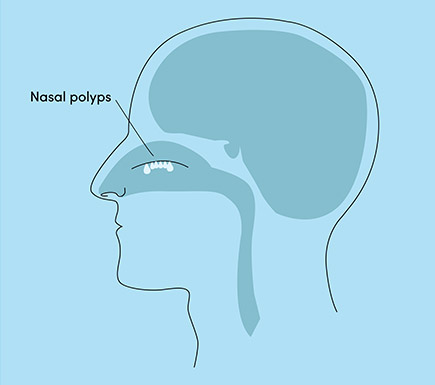
Nasal polyps are benign growths in the nose, causing breathing issues, smell loss and congestion. This is typically due to inflammation that can be managed with medication. However, severe cases may require surgical intervention.
Awards & Certifications
References
1 The crooked nose (A. BOCCIERI). Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709523/.
2 All About Dorsal Humps: Causes and Removal Options. Available: https://www.healthline.com/health/dorsal-hump.
3 Surgical Rhinoplasty. Rhinoplasty Overview International. Available: https://rhinoplastysociety.org/procedures/surgical-rhinoplasty/rhinoplasty-overview-international.

By Dr. Sam S. Rizk, M.D., FACS.
Dr. Rizk is a double board-certified facial plastic surgeon who specializes in rhinoplasty surgery and a recognized expert on the latest advances in facial plastic surgery techniques. He performs a range of facial plastic surgeries at his New York practice.




















2.jpg)