Trust Your Surgery To An Expert
Dr. Sam Rizk is a skillfully trained and experienced double-board-certified facial plastic surgeon. He consistently delivers desired revision rhinoplasty results patients expected the first time when they had their initial rhinoplasty done elsewhere!
What Is Revision Rhinoplasty?
Revision rhinoplasty1, also known as secondary rhinoplasty, is a complex surgical procedure that involves reshaping the nose to improve its appearance or function. It is often more challenging than primary rhinoplasty due to scarring and other changes that may have occurred after the initial surgery.
During the secondary nose job, Dr. Rizk may need to adjust underlying cartilage or bone structures, remove excess tissue, and graft new material into the nasal framework to achieve the desired aesthetic and functional results. Given the complexities of a NYC revision rhinoplasty procedure, it is highly important you choose a board-certified surgeon with experience.

Revision Rhinoplasty Before and After
*Results may vary.
See More ResultsQuick Guide to Revision Rhinoplasty
Preparing for Revision Rhinoplasty
Since you’ve already experienced nose surgery, you should have an idea of what to expect although Dr. Rizk will explain each step of the procedure during your consultation. To ensure your desired results are achieved, you must follow his pre-, and post-surgery guidelines. These may include:
- Stopping any medications as directed by Dr. Rizk.
- No smoking or alcohol consumption
- Expect pre-surgery testing such as blood tests and X-rays
- Creating a recovery space in your home
- Arranging for someone to drive you home after your surgery
- No strenuous activities for several weeks and at least one-week downtime
- Follow-up appointments for splint and tube removal
- Have realistic expectations and understand that it can take up to 12 months for your new nose to heal completely
You will be sedated throughout your procedure to ensure your comfort and safety. Dr. Rizk will discuss your unique treatment plan with you in great detail. He will use the best revision rhinoplasty technique to address both aesthetic and functional concerns.
Video Testimonials
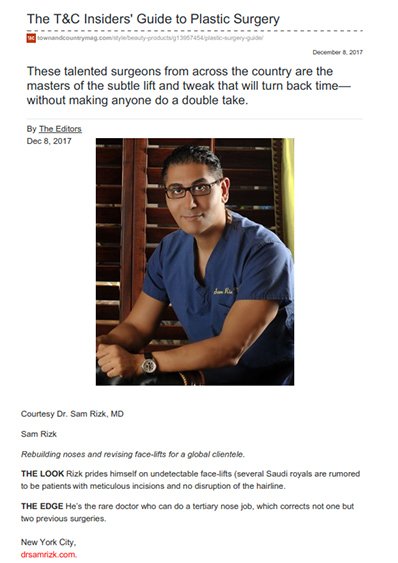
Dr. Rizk in the Media
Types of Deformities Addressed in Revision Rhinoplasty
Below are explanations of some of the most common deformities addressed in revision procedures.
What is it?
This type of nasal deformity is characterized by an inverted V-shaped shadow in the area of the middle vault of the nose.
How it occurs
Overresection of the upper lateral cartilage, the cartilage that forms the sides of the nose’s bridge. It often occurs when the surgeon who performed the original procedure made a mistake during the removal of a nasal bump and during the fracturing of the nasal bones (this destabilizes the upper lateral cartilage).
How to correct it
Dr. Rizk prefers surgery to fillers because fillers do not fix the deformity permanently. The volume gained through hyaluronic acid-based fillers, for instance, lasts for about six months. Fillers are also less precise than surgery and can make the nose look larger. Moreover, they can cause inflammation and scar tissue, which makes a later surgery more difficult to perform. Finally, fillers can move around inside the nose. Therefore, he favors surgery to fillers when correcting an inverted V deformity. The surgery often involves the placement of dorsal cartilage above the nasal bridge to narrow the nose and widen the middle nasal vault.
Transform Your Look With Revision Rhinoplasty Surgery
Revision rhinoplasty with Dr. Rizk in New York City begins with a discussion of your goals, preferences, and concerns. Drawing on extensive facial plastic surgery experience, Dr. Rizk understands your lost trust, focusing on restoring confidence by achieving the look you originally envisioned while ensuring balanced functionality.
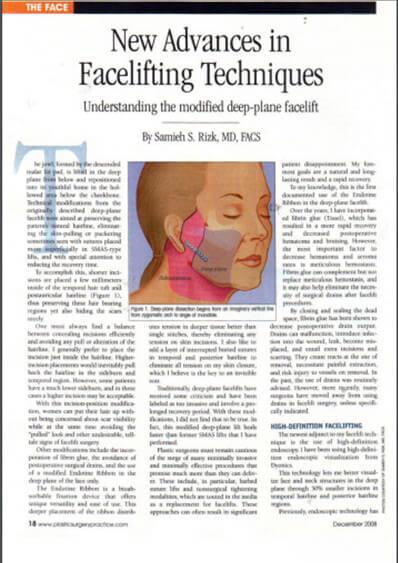
Revision rhinoplasty is more intricate than a primary procedure due to scar tissue, altered nasal structures, and potential cartilage deficiencies from previous surgery. Dr. Rizk employs advanced techniques, including meticulous dissection and structural restoration, to refine aesthetics and improve function. His precision-driven approach prioritizes patient safety, comfort, and natural-looking results.
Understanding Recovery Times
Typically, revision rhinoplasty with Dr. Rizk offers a more streamlined recovery compared to a primary nose job, as his refined approach minimizes post-operative challenges. To support healing and reduce infection risk, Dr. Rizk may prescribe specific medications and antibiotics.
You can expect to experience less bruising and swelling than you may have experienced with your primary nose job. It is important to follow Dr. Rizk’s personalized rhinoplasty recovery guidelines and instructions to ensure minimal discomfort during your recovery. You will need to take at least one week off and may resume your usual activities two weeks post-surgery.
As with your first nose job, it can take up to twelve months for your nose to completely recover and heal from the procedure. Contact Dr. Rizk’s office if you have any concerns or questions during your recovery period.
Am I a Candidate for Revision Rhinoplasty?
Unfortunately, not everyone is a suitable candidate and some deformities can’t be corrected. Your suitability depends on the objective of your initial nose job surgery and the outcome.
Important factors that Dr. Rizk considers include:
- The integrity of the skin
- How much cartilage was removed in the original procedure
- How much scar tissue there is
- The extent of the deformity and whether you need grafting
It is important to have realistic expectations and consult with a rhinoplasty specialist who is experienced in revision rhinoplasty procedures4 to ensure the best possible outcome.
Associated Risks and Complications
All surgical procedures present possible risks and complications. Dr. Rizk is a double-board-certified surgeon with many years of experience. His skills, experience, and knowledge greatly reduce associated risks which are similar to those experienced during a primary rhinoplasty.
Why Consult Dr. Rizk for NYC Revision Rhinoplasty?
Dr. Rizk brings decades of experience and artistic insight to revision rhinoplasty. He understands the fear, distrust, and anxiety that often follows a failed surgery, and he is dedicated to offering compassionate guidance. With a precise, methodical approach and advanced techniques, he works closely with each patient to restore confidence and achieve results.
Dr. Rizk is a highly sought after facial plastic surgery specialist who has developed an impressive reputation in rhinoplasty surgery thanks to his commitment to excellence and patient-centered care. Schedule a consultation today with Dr. Rizk today to unlock your full potential.
Frequently Asked Questions
How much does revision rhinoplasty cost?
The exact cost of a revision rhinoplasty will vary depending on how complex the surgery is and the individual patient’s needs. Generally, secondary rhinoplasty will be more expensive than primary rhinoplasty due to its complexity and the amount of reconstructive work that may be necessary.
Is revision rhinoplasty dangerous?
Secondary rhinoplasty is a much more complex procedure than primary rhinoplasty, and as with any kind of surgery, there are risks. However, these risks are minimized when you work with an experienced board-certified plastic surgeon.
What can secondary rhinoplasty fix?
Secondary rhinoplasty can help improve facial symmetry by refining the nasal tip shape or size, changing the bridge’s projection, and reducing alar flaring or narrowing wide nostrils. It can straighten a crooked nose or create smoother curves across the surface. Importantly, revision nose jobs often address what wasn’t fixed during the initial surgery.
How soon after my primary nose job can I have secondary rhinoplasty?
It is generally ill-advised to receive revision rhinoplasty before the patient has completely recovered from the initial surgery (6-12 months), and the true results can be seen. It is very important to have realistic expectations when choosing to undergo secondary rhinoplasty. A patient’s idea of perfection is often impossible to satisfy, and further operation on an altered nose can result in more unwanted stress for the patient, both physically and emotionally. The nose is one of the most prominent features on the face and it controls how elongated or wide a face may appear. Reconstructive surgeries should not be mistaken as a method of gaining self-confidence. Before recommending the procedure to you, Dr. Rizk will do a thorough assessment to see if you are a suitable candidate for revision rhinoplasty.
What happens if I live far from the New York area?
Dr. Rizk has had patients come in from around the world to see him, and creates special plans to ensure a safe and effective travel plan and surgery. Do not be discouraged if you live outside of the immediate New York area – there is no substitute for the expertise and capabilities you will find with Dr. Sam Rizk. He has worked on hundreds of patients from various cultures and understands how best to complement the nose to the face. Contact his office today to determine if you are a suitable candidate for a revision rhinoplasty with Dr. Rizk.
Awards & Certifications
References
1 Facial Plastic and Reconstructive Surgery. Revision Rhinoplasty. Available: https://med.stanford.edu/drmost/aesthetic-services/procedures/revision-rhinoplasty.html.
2 Rhinoplasty Society. Revision Rhinoplasty | Secondary Rhinoplasty. Available: https://rhinoplastysociety.org/procedures/surgical-rhinoplasty/secondary-rhinoplasty-international.
3 Stefan Hacker, Jonathan Pollock, Wolfgang Gubisch, Sebastian Haack. Differences between Primary and Revision Rhinoplasty: Indications, Techniques, Grafts, and Outcomes. Available: https://pubmed.ncbi.nlm.nih.gov/34270514/.
4 American Society of Plastic Surgeons. Understanding revision rhinoplasty and why patients seek out this procedure. Available: https://www.plasticsurgery.org/news/blog/understanding-revision-rhinoplasty-and-why-patients-seek-out-this-procedure.
5 American Society of Plastic Surgeons. Rhinoplasty. What are the risks of rhinoplasty? Available: https://www.plasticsurgery.org/cosmetic-procedures/rhinoplasty/safety.

By Dr. Sam S. Rizk, M.D., FACS.
Dr. Rizk is a double-board-certified facial plastic surgeon who specializes in rhinoplasty surgery and is a recognized expert on the latest advances in facial plastic surgery techniques. He performs a range of facial plastic surgeries at his New York practice.






















2.jpg)